(Effet de l’épaisseur de la résine composite sur la résistance au cisaillement de la liaison à la dentine)
• Richard B. Price, DDS, MS, MRCD(C), FDS RCS
(Edin) •
• Gorman Doyle, DDS, MS •
• Darcy Murphy, B.Sc. •
Les fabricants de certaines résines composites postérieures condensables
prétendent que leurs produits peuvent
être appliqués «en vrac» et photopolymérisées par couches de 5 mm d’épaisseur.
Cette étude vise à comparer la résistance au cisaillement de trois résines composites
liées à la dentine par couches progressives, respectivement de 2 et de 5 mm
d’épaisseur. En général, la résistance est compromise par l’épaisseur de la
résine composite (p < 0,0001). Quant à celle de chaque résine composite évaluée,
elle est très largement inférieure lorsque la résine est photopolymérisée par couches
de 5 mm plutôt que de 2 mm (p < 0,0005). Les deux résines composites
condensables évaluées ont affiché une résistance au cisaillement inférieure aux
résines composites classiques lorsqu’elles sont photopolymérisées par couches de 5
mm (p < 0,01).
Mots clés MeSH : composite resins; dental bonding; dentin-bonding systems
© J Can Dent Assoc 2000; 66:35-9
Cet article a fait l’objet d’une révision par des pairs.
Some manufacturers claim1,2 that their high viscosity condensable posterior composites can be successfully light-cured in up to 5-mm-thick increments. The maximum recommended curing depth for a conventional composite (e.g., Z100, 3M Dental, St. Paul, MN]) is 2 mm to 2.5 mm.3 As light passes through composite, the light is absorbed or scattered and the light intensity is reduced as the composite thickness increases. It has been previously reported4,5 that the composite-dentin bond strength decreases as the amount of light energy decreases. Consequently, if insufficient light passes through a 5-mm increment of composite, then the composite-dentin bond may be reduced. Single Bond (3M Dental, St. Paul, MN), Bond 1 (Jeneric/Pentron, Wallingford, CT) and Solo (Kerr Corporation, Orange, CA) dentin bonding systems (DBS) can generate 24-hour shear bond strengths greater than 18 MPa,6-8 but the composite specimens were not polymerized in a 5-mm increment. Also, gelatin capsules were used, allowing additional light to reach the resin-dentin interface from the sides of the capsule and thereby increasing the bond strength.
The hardness at the bottom of 4 mm of conventional composite has been reported to be less than the hardness at the top,9,10 and at 3 mm the degree of conversion at the bottom of the composite is about 50% of that at the top of the composite.11 Inadequate curing of the composite not only adversely affects its physical properties,12 but also increases its cytotoxicity.13 Consequently, it is recommended that conventional composites be light-polymerized in increments no greater than 2-mm thick.10,11,14
This study compared the 24-hour in-vitro shear bond strengths of 2-mm and 5-mm increments of two condensable and one conventional composite resin when bonded to dentin. The hypotheses were that there would be no difference in the bond strengths obtained from the 2-mm and 5-mm specimens of the condensable composites and that the 5-mm specimens of condensable composites would have greater bond strengths than the 5-mm specimens of conventional composite.
Materials and Methods
Ninety extracted human molar teeth were collected and stored in aqueous
0.5% w/v chloramine-T-hydrate7 (Lot # 07117AG, Aldrich Chemical Co., Milwaukee,
WI) at 4ºC to 6ºC. Before the dentin surfaces were prepared, the teeth were thoroughly
washed under running water for 24 hours. The teeth were then mounted in acrylic resin such
that only about half of the tooth was embedded in the resin and the buccal surfaces
protruded well above the resin. This positioning avoided any possible contamination of the
dentin surface by resin when the buccal surface was ground flat. To produce consistent
bonding conditions, the buccal surfaces of the teeth were ground flat against a
water-cooled abrasive wheel using a sequence of fresh 120-, 240- and 400-grit silicon
carbide papers. Since dentin depth and tubule orientation have been shown to affect bond
strengths and resin penetration,15,16 the teeth were ground to approximately
the same depth halfway between the dentoenamel junction and the pulp. This depth was
considered to most accurately represent the depth of a typical cavity preparation and thus
was a representative site to test resin-dentin bond strengths. The teeth were inspected to
ensure that there was no enamel or pulpal exposure at the bonding site. The teeth were
then randomly coded and stored in water 4ºC to 6ºC. Final finishing with fresh 600-grit
silicon carbide paper was done 1 to 4 hours before bonding. The teeth were then stored in
water at 37ºC ± 1ºC. Each bonding system was used in accordance with the
manufacturer’s instructions.1-3 All of the bonding systems were used on
moist dentin, and excess surface water was removed by blotting the edges of the tooth with
a KimWipe. During the bonding procedure, the teeth were kept at 34ºC ± 2ºC to mimic the
intraoral environment. Distilled water at 35ºC ± 2ºC was used to thoroughly rinse off
the gel etchant.
 |
| Fig 1 Schematic of the metal moulds used to produce 2- and 5 - mm thick composite resin cylinders |
All of the dentin surface was treated with the DBS, but the dentin bonding adhesives were light-cured only within the metal mould over the dentin to which the composite was subsequently bonded. One conventional composite (Z100, Lot # 19981105 & 19980702) and two condensable composites (Prodigy Condensable [Lot # 810876, Kerr Corporation, Orange, CA] and Alert [Lot # 17020, Jeneric/Pentron, Wallingford, CT]) were used with their respective bonding systems (Single Bond, Lot # 7AD, 7BA; Solo, Lot # 810578; and Bond 1, Lot # 811931). The composite was packed into either a 2-mm-high or a 5-mm-high split metal mould (Fig. 1) and bulk-cured from the top of the mould for 40 seconds using a Demetron 401 (Serial # 4732765, Demetron/Kerr, Danbury, CT) curing light. This light had an 80-watt bulb and an 11-mm curing light tip. The power output from the curing light was monitored every 20 samples to ensure adequate power output. In accordance with manufacturer’s instructions,1 a 0.5-mm-thick layer of Flow It Shade A1 (Jeneric/Pentron, Wallingford, CT) was applied to the dentin within the mould and light-cured for 40 seconds before the Alert composite was placed in the mould.
Immediately after the composite had been light-cured for 40 seconds, the mould was carefully removed and the specimen placed in 37ºC ± 1ºC water. When one 2-mm and one 5-mm specimen had been made with one composite, two specimens were made with the next composite. This sequence was repeated until 15 specimens had been made for all six combinations of 2-mm-thick and 5-mm-thick composites, a total of 90 specimens.
24-Hour Shear Bond
Strength Testing
After bonding, the samples were stored in 37ºC ± 1ºC distilled water for
at least 16 hours before and 2 hours after thermo cycling. The teeth were thermocycled 100
times17 from 5ºC to 55ºC with a 30-second dwell time and a 30-second
intermediate time at ambient temperature of 21ºC, a total of 200 minutes. They were
debonded in a water bath at 37ºC ± 1ºC using an Instron 1000 (Instron, Canton, MA) in a
shear bond strength test mode in the same sequence in which they were made. A measured
crosshead speed of 2.8 mm/min. was used, which was within the 1 mm/min. to 5 mm/min. range
used by other researchers.4-8,15,16,18
The effects of the three different bonding systems, the different composites and the different composite thicknesses were compared for bond strength using ANOVA and a pairwise t-test on differences between least squares means, with levels adjusted according to SIDAK’s inequality for all main effect least squares means.19
Examination of Debonded Specimens
 |
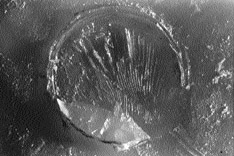 |
| Figure 2: Example of an adhesive failure between the dentin and the composite. | Figure 3: Example of a mixed failure with composite left on the dentin. |
The debonded dentin surfaces were coded and examined in a random sequence using a light microscope at 40X magnification. The mode of failure of the DBS was recorded as either “adhesive,” meaning none or very little (< 30%) composite still remaining on the dentin surface (Fig. 2), or “mixed,” meaning composite remaining on > 30% of the dentin surface (Fig. 3), or “dentin fracture,” meaning dentin fractured with composite resin attached to a portion of the fractured dentin.
Results
The mean light intensity output for the Demetron 401 curing light was 700 mW/cm2.
The composite buttons were 4.22 mm in diameter, with a mean height of 2.01 ± 0.12 mm and
4.98 ± 0.15 mm.
ANOVA showed that the composite and composite thickness had a significant effect on the bond strength results (p < 0.0001)
Table 1 Two-way ANOVA table for the effect of composite and thickness on bond strength
| DF | Sum of Square | Mean Square | f Value | p Value | Power | |
| Composite | 2 | 1242.68 | 621.34 | 79.12 | <0.0001 | 1.0 |
| Thickness (mm) | 1 | 2592.42 | 2592.42 | 330.10 | <0.0001 | 1.0 |
| Composite * Thickness (mm) | 2 | 483.99 | 242.00 | 30.81 | <0.0001 | 1.0 |
| Residual | 84 | 659.99 | 7.85 |
(Table 1). Of the 5-mm-thick specimens, the pairwise t-test on differences between least squares means showed that the Alert (3.9 MPa) and Prodigy Condensable (6.5 MPa) had the lowest bond strengths and Z100 had the greatest bond strength (16.8 MPa) (Table 2). Of the 2-mm-thick specimens, Z100 (21.3 MPa) and Prodigy Condensable (22.2 MPa) had the greatest bond strengths. All the 2-mm specimens produced greater bond strengths than the 5-mm specimens made using the same materials (p < 0.0005). The hypotheses of this study were therefore rejected, because the shear bond strengths of the 5-mm specimens were significantly lower than those of the 2-mm specimens, and the shear bond strengths of the condensable composites were not greater than those of the conventional composite.
Table 2 Mean (± SD) 24-hour shear bond strength (MPa) for 2- and 5-mm thick bulk polymerized composites
Bonding System/Composite |
Thickness | MPa ± SD |
| Solo/Prodigy Condensable | 2 mm | 22.2 ± 2.9 |
| Single Bond/Z100 | 2 mm | 21.3 ± 3.1 |
| Single Bond/Z100 | 5 mm | 16.8 ± 3.1 |
| Bond 1/Alert | 2 mm | 16.0 ± 2.5 |
| Solo/Prodigy Condensable | 5 mm | 6.5 ± 2.0 |
| Bond 1/Alert | 5 mm | 3.9 ± 3.1 |
n = 15 teeth per group, thermocycled 100x, 5º-55ºC
= Not significantly different (p = 0.01) Pairwise t-test: SIDAK
The modes of failure are shown in Table 3. Nine dentinal fractures occurred with the 2-mm increment of Z100 and four dentin fractures occurred with 2 mm of Prodigy Condensable. The mean bond strength at which all the observed adhesive failures, mixed failures and dentin fractures occurred were 4.9 ± 5.6 MPa, 13.2 ± 7.0 MPa and 23.1 ± 3.9 MPa, respectively.
Table 3 Mode of failure
Number of Failures |
Mean MPa | |||
| Composite/Thickness | Adhesive | Mixed | Dentin Fracture | |
| Prodigy Condensable 2 mm | 11 | 4 | 22 | |
| Z100 2 mm | 6 | 9 | 21 | |
| Z100 5 mm | 2 | 13 | 17 | |
| Alert 2 mm | 15 | 16 | ||
| Prodigy Condensable 5 mm | 1 | 14 | 7 | |
| Alert 5 mm | 1 | 14 | 4 | |
n = 15 samples per group
Discussion
This study attempted to standardize the testing conditions and wherever
possible mimic the intraoral environment, because in vitro laboratory testing under normal
conditions does not always reflect what happens intraorally. For example, changing the in
vitro test temperature and humidity from 23ºC/52% relative humidity (RH) to 37ºC/95% RH
has been shown to decrease the bond strength of Scotchbond Multipurpose to dentin.20
Realizing that the intraoral temperature varies depending on the location of the tooth in
the mouth and the use of a rubber dam, all bonding procedures were conducted at 34ºC ±
2ºC, which was estimated to be the temperature of teeth intraorally when bonded using a
rubber dam,21 and the specimens were debonded at 37ºC. Although many dentin
bonding studies do not thermal cycle22 the specimens, it has been shown that
thermocycling may affect bond strength.23,24 Therefore, this study used
thermocycling to mimic the 24-hour intraoral environment. The specimens were thermocycled
100 times (a total of 200 minutes), since more than 100 cycles have been shown to be
unnecessary.25
In some previous studies,4,6,7,18,26 the entire dentin surface was treated with the DBS and light-cured before the composite was bonded to the dentin. This technique has been reported to artificially increase bond strength values.27 Therefore, in this study, the DBS on the dentin surface was light-cured only within the metal mould positioned over the dentin to which the composite was subsequently bonded.
The manufacturers of Solo, Bond 1 and Single Bond recommend that after the dentin is etched and washed, the dentin should be left moist or blot dried. Some bonding systems have been shown to have increased bond strength with wet, moist or physiologically hydrated etched dentin26,28 compared to air-dried dentin. Even a brief three-second period of air drying has been shown to have a detrimental effect on the bond strength compared to the use of hydrophilic cotton pellets or KimWipes.26,28 Therefore, the dentin specimens were blot dried using KimWipes before applying the DBS. Z100 was chosen as the representative control composite, as it was the most popular composite used in dental schools in North America in 1997.29
When DBS fail mainly because of dentin fractures or cohesive composite failures, this may indicate good adhesion between the dentin and the composite.22,23 The 5-mm-thick specimens exhibited only adhesive failures and their bond strengths were significantly lower than the 2-mm results. There were more dentin fractures and mixed failures for the systems with the higher bond strengths (Table 3), and the mean overall bond strength at which all the dentin fractures occurred was 23.1 MPa. This result supports the view that bond strength and mode of failure may be related.22,23
The top of the 5-mm Alert and the Prodigy Condensable composite samples appeared to be harder than the bottom when the specimens were scraped with a sharp blade, indicating that the Alert and Prodigy Condensable composites were not adequately polymerized at the bottom. This finding supports previous reports that there is a marked decrease in hardness and degree of conversion when the composite is more than 3 mm thick.9-11,30 It may explain why the bond strengths of the 5-mm-thick condensable composites (Table 2) were surprisingly low compared to the 2-mm-specimen results, which were obtained using exactly the same materials and bonding procedure.
The manufacturer of Alert recommends1 that the composite be polymerized for 40 seconds with a light intensity greater than 400 mW/cm2 to ensure that the composite is polymerized. The curing light used in this study delivered almost twice the amount of light energy than is produced by the curing lights of about half of dental offices.31 Each composite specimen received approximately 28,000 mJ/cm2 of light energy (40s X 700 mW/cm2) from an 11-mm light tip that completely covered the 4-mm diameter composite specimen. This amount of light energy was much more than the minimum recommended and should have been adequate for all the bonding procedures, since it has been reported that there was no significant increase in top or bottom hardness when a 3.5-mm-thick specimen of Pertac (ESPE, Norristown, PA) was exposed to more than 17,000 mJ/cm2 of energy.32 However, the present research shows that considerably more light energy may be required to polymerize the bottom of a 5-mm-thick specimen of composite.
When composite in a tooth is being polymerized, some additional light may be transmitted through the tooth to polymerize the composite, but the amount of light will vary according to the tooth thickness, the tooth colour, the presence or absence of a metal matrix band and the presence or absence of metallic restorations. The 2- and 5-mm metal moulds used in this study did not allow light to penetrate the composite from the side and allowed light to enter the specimen only from the top. This provided a true test of the manufacturer’s claims1,2 that the composite can be polymerized in a 5-mm-thick increment, for it is known that the depth of cure is significantly greater when a white mould that allows light penetration from the sides is used compared to a stainless steel or a black mould.33 To maximize light penetration through 5 mm of composite, lighter shades of composite were used (A1 for Z100, A1 for Prodigy Condensable and A2 for Alert) since it has been reported that darker shades require increased light exposure.14,30,33,34 Since inadequate light intensity adversely affects bond strength,4,5 the bond strengths may be even lower when darker shades are used (e.g. A3.5 for Alert or A3 for Prodigy Condensable). Further research is required to determine the relationship between shade, filler content, light transmission through the composite, hardness, degree of conversion and bond strength, because the bottom of the 5-mm Z100 conventional composite appeared to be harder than the condensable composites, and this product had the greatest 5-mm bond strength.
Although it could be suggested that the composite resin will eventually polymerize at the base of the restoration, the initial low bond strength may be inadequate to resist the polymerization shrinkage of the composite and thus prevent failure of the bond to the dentin when the patient chews on the restoration. Bond failure may cause increased microleakage at the bottom of a 5-mm bulk polymerized Class II proximal box and increased cytotoxicity13 from the inadequately polymerized composite resin.
Because the shear bond strengths of the 5-mm specimens were significantly lower than those of the 2-mm specimens and the shear bond strengths of the condensable composites were not greater than those of the conventional composite, clinicians should not try to bond 5-mm increments of composite to dentin.
Conclusions
Two conclusions were drawn. First, the shear bond strengths to dentin of Z100,
Alert and Prodigy composites tested were much lower when cured in a 5-mm increment than
when cured in a 2-mm increment of composite (p < 0.0005). Second,
the condensable composites tested did not have a greater bond strength to dentin than the
conventional composite when polymerized in a 5-mm bulk increment (p < 0.01).
Acknowledgments
The authors thank Dr. P. Andreou, biostatistician, Dalhousie University, for
conducting the statistical analyses. The composites were kindly donated by the
manufacturers and the study was supported by the Dalhousie University Alumni Oral Health
Research Fund.
Dr. Price is associate professor in the department of dental clinical sciences of the faculty of dentistry, Dalhousie University.
Dr. Doyle is assistant professor in the department of dental clinical sciences of the faculty of dentistry, Dalhousie University.
Mr. Murphy is a dental student, Dalhousie University.
Reprint requests to: Dr. B. Richard Price, Department of Dental Clinical Sciences, Faculty of Dentistry, Dalhousie University, Halifax NS B3H 3J5
The authors have no declared financial interest in any company manufacturing the types of products mentioned in this article.
References
1. Alert and Bond 1 Product Instructions. Jeneric/Pentron Inc. Wallingford, CT.
2. Prodigy Condensable and Solo Product Instructions. Kerr USA. Orange, CA.
3. Z100 and Single Bond Product Instructions. 3M Dental Products. St. Paul, MN.
4. Hinoura K, Miyazaki M, Onose H. Effect of irradiation time to light-cured resin composite on dentin bond strength. Am J Dent 1991; 4:273-6.
5. Miyazaki M, Hinoura K, Onose H, Moore BK. Influence of light intensity on shear bond strength to dentin. Am J Dent 1995; 8:245-8.
6. Latta MA, Shaddy RS, Barkmeier WW. Laboratory evaluation of one-component dental adhesives. J Dent Res 1999; 78(IADR Abstract #3427):534.
7. Swift EJ Jr, Bayne SC. Shear bond strength of a new one-bottle dentin adhesive. Am J Dent 1997; 10:184-8.
8. Hammesfahr PD, Sang J, Hayes LC. In-vitro dentin shear bond strength study of various adhesives. J Dent Res 1999; 78(IADR Abstract #3431):534.
9. Vargas MA, Cobb DS, Schmit JL. Polymerization of composite resins: argon laser vs. conventional light. Oper Dent 1998; 23:87-93.
10. Hirabayashi S, Hood JA, Hirasawa T. The extent of polymerization of Class II light-cured composite resin restorations; effects of incremental placement technique, exposure time and heating for resin inlays. Dent Mater J 1993; 12:159-70.
11. Rueggeberg FA, Caughman WF, Curtis JW Jr, Davis HC. Factors affecting cure at depths within light-activated resin composites. Am J Dent 1993; 6:91-5.
12. Baharav H, Brosh T, Pilo R, Cardash H. Effect of irradiation time on tensile properties of stiffness and strength of composites. J Prosthet Dent 1997; 77:471-4.
13. Caughman WF, Caughman GB, Shiflett RA, Rueggeberg F, Schuster GS. Correlation of cytotoxicity, filler loading and curing time of dental composites. Biomaterials 1991;12:737-40.
14. Kanca J 3rd. The effect of thickness and shade on the polymerization of light-activated posterior composite resins. Quintessence Int 1986; 17:809-11.
15. Wakefield CW, Draughn RA, Sneed WD, Davis TN. Shear bond strengths of six bonding systems using the pushout method of in vitro testing. Oper Dent 1998; 23:69-76.
16. Yoshiyama M, Carvalho RM, Sano H, Horner JA, Brewer PD, Pashley DH. Regional bond strengths of resins to human root dentine. J Dent 1996; 24:435-42.
17. Fitchie JG, Puckett AD, Reeves GW, Hembree JH. Microleakage of a new dental adhesive comparing microfilled and hybrid resin composites. Quintessence Int 1995; 26:505-10.
18. Meiers JC, Shook LW. Effect of disinfectants on the bond strength of composite to dentin. Am J Dent 1996; 9:11-4.
19. Sidak, Z. Rectangular confidence regions for the means of multivariate normal distributions. J Am Statistician Assoc 1967; 62:626-33.
20. Nystrom GP, Holtan JR, Phelps RA 2nd, Becker WS, Anderson TB. Temperature and humidity effects on bond strength of a dentinal adhesive. Oper Dent 1998; 23:138-43.
21. Spierings TA, Peters MC, Plasschaert AJ. Surface temperature of oral tissues. A review. J Biol Buccale 1984; 12:91-9.
22. Al-Salehi SK, Burke FJ. Methods used in dentin bonding tests: an analysis of 50 investigations on bond strength. Quintessence Int 1997; 28:717-23.
23. Øilo G, Austrheim EK. In vitro quality testing of dentin adhesives. Acta Odontol Scand 1993; 51:263-9.
24. Miyazaki M, Sato M, Onose H, Moore BK. Influence of thermal cycling on dentin bond strength of two-step bonding systems. Am J Dent 1998; 11:118-22.
25. Burger KM, Cooley RL, Garcia-Godoy F. Effect of thermocycling times on dentin bond strength. J Esthet Dent 1992; 4:197-8.
26. Kanca J 3rd. Wet bonding: effect of drying time and distance. Am J Dent 1996; 9:273-6.
27. Van Noort R, Cardew GE, Howard IC, Noroozi S. The effect of local interfacial geometry on the measurement of the tensile bond strength to dentin. J Dent Res 1991; 70:889-93.
28. De Goes MF, Pachane GC; Garcia-Godoy F. Resin bond strength with different methods to remove excess water from the dentin. Am J Dent 1997; 10:298-301.
29. Mjör IA, Wilson NH. Teaching Class I and Class II direct composite restorations: results of a survey of dental schools. JADA 1998; 129:1415-21.
30. Curtis JW Jr, Rueggeberg FA, Lee AJ. Curing efficiency of the Turbo Tip. Gen Dent 1995; 43:428-34.
31. Martin FE. A survey of the efficiency of visible light curing units. J Dent 1998; 26:239-43.
32. Koran P, Kürschner R. Effect of sequential versus continuous irradiation of a light-cured resin composite on shrinkage, viscosity, adhesion, and degree of polymerization. Am J Dent 1998; 10:17-22.
33. Harrington E, Wilson HJ. Depth of cure of radiation-activated materials — effect of mould material and cavity size. J Dent 1993; 21:305-11.
34. Myers ML, Caughman WF, Rueggeberg FA. Effect of restoration composition, shade, and thickness on the cure of a photoactivated resin cement. J Prosthodont 1994; 3:149-57.