Critères de restauration des dents traitées par endodontie
Alex McLean, DMD, B.Sc. (Eng.)
SOMMAIRE
Dans cet article, on indique les critères qui permettent au clinicien de déterminer si les dents traitées par endodontie peuvent être restaurées à un haut degré de prévisibilité. Le but de cet article n’est pas d’empêcher qu’on restaure les dents qui ne répondent pas à ces critères. Il offre, au contraire, une méthode scientifique d’identification des dents qui, lorsqu’on les restaure, présentent une forte probabilité de succès à long terme.
Pour une dent traitée par endodontie qui ne nécessite pas un tenon, il faut 4,5 mm de dent solide au-dessus de l’os et une dentine d’au moins 1 mm d’épaisseur après la préparation. Pour une dent nécessitant un tenon, il faut en outre une racine assez longue pour permettre 4 mm de gutta percha apicale non touchée et une longueur de tenon égale à celle de la couronne.
Il est essentiel d’évaluer les charges fonctionnelles auxquelles la dent restaurée sera soumise. Il convient d’éviter de se servir des dents traitées par endodontie comme piliers soutenant une PPA avec un attachement de précision, une PPA avec une extension distale ou une PPF à cantilever.
Mots-clés MeSH: dental prosthesis design; post and core technique; tooth, non-vital/therapy.
© J Can Dent Assoc 1998; 64:652-6
Cet article a fait l'objet d'une révision par des pairs.
[
Introduction | Supra-Bony Tooth Structure | Biologic Width | The Ferrule Effect | Intact Anterior Teeth | Posterior and Anterior Teeth Requiring Crowns | Thickness Of Coronal Tooth Structure | The Need For a Post | Apical Seal | Post Length | What Loads Will the Restored Tooth Experience | Criteria For Successful Restoration | Discussion | Acknowledgements | References ]
The restoration of the endodontically treated tooth is an important aspect of dental practice involving a range of treatment options of varying complexity. The clinician must be able to predict the probability of restoring such teeth successfully.
Generally, endodontically treated teeth have experienced significant coronal destruction as well as a loss of radicular dentin, secondary to endodontic treatment. There is evidence that these teeth have a reduced level of proprioception1,2 which could impair normal protective reflexes. Successful management requires an assessment of the role of the restored tooth in the overall dentition, the load it will have to bear and the status of adjacent teeth. Compromise treatments may have to be considered, due to the cost of treatment or patient discomfort.
The intent of this article is to present a set of criteria which, when met, will indicate a predicably restorable endodontically treated tooth.
The bulk of supra-bony tooth structure is the most critical factor determining the restorative prognosis for a tooth.3 There have been suggestions that endodontically treated teeth are somehow more “brittle” than vital teeth. Research by Helfer4 et al has shown decreased moisture content in the dentin of pulpless teeth, the significance of which is not clear.
Huang and Schilder5 have shown that the modulus of elasticity (Young’s modulus) and the ultimate strength of dentin increase as it dehydrates (i.e. it becomes stiffer). These researchers also showed that ultimate strength in tension and compression, in both vital and non-vital dentin, is essentially identical. Interestingly, they found that Young’s modulus of dentin was lower in non-vital teeth than in vital teeth. This evidence does not support the idea that the mechanical properties of non-vital dentin are significantly different from those of vital dentin.
To have a healthy gingival attachment apparatus, room is required between the margin of the restoration and the crest of bone. Gargiulo et al6 found the dimensions of the attachment apparatus to range from 1.77 mm to 2.43 mm. This means that there should be an absolute minimum of 2.5 mm between the restoration margin and the crest of bone (see Fig. 1).
Fugazzotto et al7 and Freeman8 have recommended that at least 3 mm be allowed.
An adequate bulk of tooth coronal to the restoration margin is required to restore the tooth. The amount of coronal tooth structure, along with the position of the tooth in the arch, will dictate: the type of build-up indicated; whether a preformed post, or a cast post and core are indicated; and whether a crown is needed.
Fig 1: Biologic width considerations.
With the placement of a crown on a tooth the “ferrule effect” must be considered. A ferrule is an encircling band of cast metal that acts as a reinforcing sleeve around the coronal portion of the tooth. Tjan and Whang,9 using a short 60 degree collar, found that this collar did not increase resistance to root fracture. Other studies, such as those of Barkhordar et al10 and Sorensen and Engelman,11 have shown that ferrules confer significant increases in resistance to fracture. The differences stem from a range of interpretations about what constitutes a ferrule.
Sorensen and Engelman11 define the ferrule effect as a “360 degree metal collar of the crown surrounding the parallel walls of the dentin extending coronal to the shoulder of the preparation. The result is an elevation in resistance form of the crown from the extension of dentinal tooth structure.” Barkhordar et al10 used a 2-mm long ferrule wall, and Sorensen and Engelman11 a 1-mm long ferrule. Accepting that the ferrule is only effective when the walls are very close to parallel, and allowing for a somewhat rounded transition from ferrule wall to the prep margins, it seems prudent to accept 2 mm of ferrule length as a minimum clinically.
There is a consensus that there is no need to place crowns or posts in anterior teeth (incisors and cuspids) with essentially intact crowns, because posts do not reinforce endodontically treated teeth.12-15 In such teeth, closure of the access preparation with a bonded composite resin restoration is all that is required, provided the tooth meets the occlusal requirements and the patient is happy with its appearance.
Posterior and Anterior Teeth Requiring Crowns
Almost without exception, endodontically treated posterior teeth (distal to the cuspid) benefit from cuspal coverage with some form of crown.12 In addition, many anterior teeth will require crowns for esthetic, structural or occlusal reasons. For such teeth to be successfully restored, there must be a minimum of 4.5 mm of solid tooth structure above the bone crest; given that a minimum of 2.5 mm is required for biologic width and 2 mm for an effective ferrule.
Thickness Of Coronal Tooth Structure
What constitutes adequate thickness of coronal tooth structure is also a subject of some discussion. Sorensen and Engelman,11 and Tjan and Whang,9 found that increasing the thickness of axial dentin beyond 1 mm did not increase the strength of the restored tooth. Both showed, however, that with thicker axial dentin, failure was much more likely to be due to dislodgement rather than root fracture. Tjan and Whang measured the thickness of buccal dentin in their work, while Sorensen and Engelman measured the minimum dentin thickness and did not test teeth with a dentin thickness of less than 1 mm. On some teeth it is virtually impossible to obtain this 1 mm thickness of dentin in the interproximal areas, after both endodontic treatment and crown preparation. However, with careful tooth preparation it can be approached, and in the more important buccal and lingual walls it can usually be obtained.
The work of Hunter et al,16 using photoelastic models, supports the concept that preservation of coronal dentin strengthens the tooth. Apparently, thicker coronal dentin reduces the odds of failure by fracture of tooth structure and improves the odds that a failure will involve a simple dislodgement of the core. In such a case the tooth can be saved. The evidence indicates that more coronal dentin is better than less.
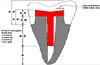
A 1 mm thickness of axial dentin seems to be the accepted minimum.17 However, this figure is empirical, based on opinion and clinical experience rather than research. This 1 mm refers to the thickness of dentin between the inside of the canal wall and the outside surface of the ferrule as shown in Fig. 2.
Endodontically treated teeth all require build-ups of some sort, if only to close the access preparation and fill the pulp chamber. Where a crown is to be placed on the tooth as a final restoration, this build-up is often called upon to provide resistance and retention form to the preparation. Retention of the build-up is often accomplished by placement of a post which engages root structure.
Nayyar et al18 and Kane et al19 have both described the use of amalgam cores as build-ups for posterior teeth retained by the pulp chamber or by extensions of amalgam into the coronal 2 mm to 4 mm of canal space. Kane et al showed that where 4 mm or more of pulp chamber height remained, there was no advantage to placing amalgam into the root canal space. In addition, even in teeth with only 2 mm of pulp chamber height left, the fracture loads were comparable to those of teeth with 4 mm high pulp chambers.19 On posterior teeth in which the core build-up can be retained by remaining pulp chamber anatomy there is no need or advantage to placement of a post.
With both anterior teeth and posterior teeth the decision to place a post is based on the answer to the question; is a post required to retain the build-up? The decision to place a post should not be based on the desire to strengthen the tooth. Sorensen and Martinoff20 found no evidence that placement of a post and/or crown on an anterior tooth has a significant effect on the prognosis of the tooth. Where a post is necessary to retain the build-up, the length of the post and the length of the remaining apical seal can greatly influence the probability of the success of the restoration.
Fig 2: Minimum dimensions for a predictably restorable tooth.
The length of apical seal remaining after post preparation and the degree to which it was disturbed during post-hole preparation can influence the long-term success of the restoration. The realities of post-hole preparation are such that, in most cases, some form of mechanical preparation of the post-hole is required.
There is support21-23 for leaving 4 mm to 5 mm of undisturbed apical gutta percha after post preparation. Various researchers 21,22,24 have reviewed different methods of post-hole preparation and none found an increase in apical leakage attributable to any particular procedure for removing gutta percha. However, Haddix et al25 found significantly less leakage when gutta percha was removed using heated pluggers. The apical seal was much better when 5 mm of gutta percha remained following post preparation, as opposed to when 3 mm remained.
The work of Ouzounian and Schilder26 shows that at a distance of 5 mm from the apex, there is a 1 mm thickness of dentin, before post preparation, only on cuspids, upper incisors, lower bicuspids and the palatal root of upper molars. There is consistently less than 1 mm of remaining dentin on all other roots. This underlines the need for careful assessment of each root prior to post preparation.
Caputo et al17 suggested that a minimum of 1 mm of sound dentin surround the apical end of the post. It is difficult, if not impossible, to measure this thickness clinically. If this recommendation was followed rigidly, the use of posts in many teeth would be ruled out. Given the high success rate shown with long posts in Sorensen and Martinoff’s retrospective study,20 thinner cross-sections of dentin apparently suffice.
Standlee et al27 showed retention of passive posts increased directly with length. Morgano28 recommends that the post be as long as possible, while maintaining adequate apical seal. Sorensen and Martinoff20 showed that where post length in the canal was equal to or greater than the length of the crown, the success rate was 97.5%, regardless of post design. The success rate was greater than 97.7% with para-post, even when shorter post dimensions were included. Ideally the length of the post extending into the root should equal the length of the crown.
What Loads Will the Restored Tooth Experience
The load borne by the restored tooth is a major indicator of the success of a restoration. Sorensen and Martinoff29 found in their retrospective study that while the success rate for single unit crowns was 94.8%, the rate was 89.2% for fixed partial denture (FPD) abutments and dropped to 77.4% for removable partial denture (RPD) abutments (both distal extension and tooth born designs). Nyman and Lindhe30 found fractures in abutment teeth occurred more frequently in root treated teeth, and primarily in root treated teeth fitted with posts, serving as terminal abutments for free end segments. Hatzikyriakos et al31 found in a three-year retrospective study that the failure rate for endodontically treated teeth used as abutments for FPDs and RPDs was over double that for teeth not used as abutments.
Testori et al32 recommended against anchoring a cantilever bridge on an abutment that was endodontically treated and fitted with a post. Testori also stated that attaching removable partial dentures with extracoronal attachments to individual endodontically treated teeth placed these teeth at significant risk. Abutment teeth for distal extension RPDs are far more likely to experience high bending stresses in a mesio-distal direction than either tooth borne or non-cantilevered FPD abutments. The stresses generated in the tooth structure by such loads can be greater that those of comparable bucco-lingual loading, as most of these abutment teeth are much narrower mesio-distally than bucco-lingually (see Fig. 3).
Based on the available data, the use of an endodontically treated tooth to support a precision attachment RPD, a distal extension RPD or a cantilevered FPD cannot be considered highly predictable. In addition, the use of root treated teeth to support non-cantilevered FPDs must be assessed carefully on an individual basis. Root treated teeth may not be suitable as abutments in individuals with a history of bruxism, or those requiring long span fixed bridges.
Fig 3: Effect of bending forces from cantelever loading.
Criteria For Successful Restoration
For the endodontically treated tooth requiring a post, the minimum length of remaining solid tooth would be the sum of biologic width (2.5 mm), ferrule length (2 mm), apical seal (4 mm) and a post length (equal to crown length), (i.e. 8.5 mm + post length beyond crown margin) (see Fig. 2).
For those teeth not requiring a post, the requirements are for biologic width + ferrule length (i.e. 4.5 mm of supra-bony solid tooth; this assumes adequate bone support to provide a clinically acceptable level of mobility). In both situations, “solid tooth” refers to dentin at least 1 mm thick after preparation.
In addition, consideration of the functional loads to be borne by the tooth is essential. Single abutments supporting precision attachment RPDs, distal extension RPDs or cantilever FPDs that are endodontically treated, or likely to be in future, should be avoided. Careful assessment of the occlusal demands and other loads, such as from fixed or removable partial dentures, must be made before restoration. Endodontically treated teeth that meet these criteria can be restored with a high degree of confidence.
There is a limited amount of research that correlates structural and endodontic failure of teeth to the types of load they experience. Studies involving a large number of teeth looking at the impact of such load factors could be an invaluable aid to assessing what will and won’t work in clinical situations. The decision to place a crown, or crown and post on anterior root treated teeth is a difficult one; current evidence is inconclusive on the value of crowns and posts in these situations. This is an area where a large well-designed study could help guide the clinician. Many teeth don’t fall within the guidelines outlined here, and yet need to be restored. There is a very real need for guidelines on restoration of these teeth and for ways to assess the level of predictability associated with such restorations.
Dr. Alex McLean is in private general practice in Kamloops, British Columbia. Reprint requests to: Dr. Alex McLean, 201-418 St. Paul St., Kamloops, BC V2C 2J6
The author has no declared financial interest in any company manufacturing the types of products mentioned in this article.
References
| 1. | Loewenstein WR, Rathkarnp R. A study on the pressoreceptive sensibility of the tooth. J Dent Res 1955; 34:287-94. |
| 2. | Randow K, Glanz PO. On cantilever loading of vital and non-vital teeth an experimental clinical study. Acta Odontol Scand 1986; 44:271-7. |
| 3. | Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent 1994; 71:565-7. |
| 4. | Helfer AR, Melnick S, Schilder H. Determination of the moisture content of vital and pulpless teeth. Oral Surg 1972; 34:661-9. |
| 5. | Huang TG, Schilder H. Effects of moisture content and endodontic treatment on some mechanical properties of human dentin. J Endod 1992; 18:209-15. |
| 6. | Gargiulo AW, Wentz F, Orbun R. Dimensions and relations of the dentogingival junction in humans. J Periodontol 1961; 32:261. |
| 7. | Fugazzotto PA, Parma-Benfenati S. Pre-prosthetic periodontal considerations. Crown length and biologic width. Quintessence Int 1984; 12:1247-56. |
| 8. | Freeman B. The biologic width periodontal - restorative considerations. Univ Tor Dent J 1990; 3:32-3. |
| 9. | Tjan HL, Whang SB. Resistance to root fracture of dowel channels with various thicknesses of buccal dentin walls. J Prosthet Dent 1985; 53:496-500. |
| 10. | Barkhordar RA, Radke R, Abbasi J. Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent 1989; 61:676-8. |
| 11. | Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent 1990; 63:529-36. |
| 12. | Guzy GE, Nicholls JI. In vitro comparison of intact endodontically treated teeth with and without end-post reinforcement. J Prosthet Dent 1979; 42:39-44. |
| 13. | Assif D, Bitenski A, Pilo R, Oren E. Effect of post design on resistance to fracture of endodontically treated teeth with complete crowns. J Prosthet Dent 1993; 69:36-40. |
| 14. | Trope M, Maltz DO, Tronstad L. Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol 1985; l:108-11. |
| 15. | Sorensen JA, Martinoff JT. Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent 1984; 51:780-4. |
| 16. | Hunter AJ, Feiglin B, Williams JF. Effects of post placement on endodontically treated teeth. J Prosthet Dent 1989; 62:166-72. |
| 17. | Caputo AA, Standlee JP. Pins and posts — Why, when and how. Dent Clin North Am 1976; 20:299-311. |
| 18. | Nayyar A, Walton RE, Leonard LA. An amalgam coronal-radicular dowel and core technique for endodontically treated posterior teeth. J Prosthet Dent 1980; 43:511-15. |
| 19. | Kane JJ, Burgess JO, and Summitt JB. Fracture resistance of amalgam coronal-radicular restorations. J Prosthet Dent 1990; 63:607-13. |
| 20. | Sorensen JA, Martinoff JT. Clinically significant factors in dowel design. J Prosthet Dent 1984; 52:28-35. |
| 21. | Mattison GD, Delivanis PD, Thacker RW, Hassell KJ. Effect of post preparation on the apical seal. J Prosthet Dent 1984; 51:785-9. |
| 22. | Camp LR, Todd MJ. The effect of dowel preparation on the apical seal of three common obturation techniques. J Prosthet Dent 1983; 50:664-6. |
| 23. | Goodacre CJ, Spoolnik KJ. The prosthodontic management of endodontically treated teeth: A literature review. Part II. Maintaining the apical seal. J Prosthodont 1995; 4:51-3. |
| 24. | Suchina JA, Ludington JR. Dowel space preparation and the apical seal. J Endod 1985; 11:11-27. |
| 25. | Haddix JE, Mattison GD, Shulman CA, Pink FE. Post preparation techniques and their effect on the apical seal. J Prosthet Dent 1990; 64:515-9. |
| 26. | Ouzounian, ZS, Schilder, H. Remaining dentin thickness after endodontic cleaning and shaping before post space preparation. Oral Health 1991; 13-5. |
| 27. | Standlee JP, Caputo AA, Hanson EC. Retention of endodontic dowels: effects of cement, dowel length, diameter, and design. J Prosthet Dent 1978; 39:401-5. |
| 28. | Morgano SM. Restoration of pulpless teeth: application of traditional principles in present and future contexts. J Prosthet Dent 1996; 75:375-80. |
| 29. | Sorensen JA, Martinoff JT. Endodontically treated teeth as abutments. J Prosthet Dent 1985; 53:631-6. |
| 30. | Nyman S, Lindhe J. A longitudinal study of combined periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol 1979; 50:163-9. |
| 31. | Hatzikyriakos AH, Reisis GI, Tsingos N. A 3-year postoperative clinical evaluation of posts and cores beneath existing crowns. J Prosthet Dent 1992; 67:454-8. |
| 32. | Testori T, Badino M, Castagnola M. Vertical root fractures in endodontically treated teeth: A clinical survey of 36 cases. J Endod 1993; 19:87-90. |