
three years after placement. The author did not provide the requisite 2-mm occlusal reduction.
• William H. Liebenberg, B.Sc., BDS •
© J Can Dent Assoc 1999; 65:582-4
[Restoravtive Intrgrity in Perspective |A Shift in Memtality|Deferred Definitive Treatment |Clinical Reality of Treatment Selection|Conculsion |References]
 |
| Figure 1: Fractured all-ceramic crown three years after placement. The author did not provide the requisite 2-mm occlusal reduction. |
The esthetic and conservative appeal of adhesive dentistry has led to overambitious applications as patients are increasingly demanding tooth-coloured restorations. Clinicians are resorting to adhesive techniques in a variety of situations that are not always appropriate, regardless of the fact that there is no scientific validation of the durability of these extended applications. Direct posterior composites, indirect partial coverage, single and multiple span anterior and posterior tooth-coloured options should be considered “probationary,” as clinical experience (Fig. 1) has revealed that a restoration’s initial esthetic appearance does not guarantee durability and maintenance of quality.1
It can be a challenge to choose the most appropriate restorative treatment. Often practitioners find themselves vacillating between traditional treatment and probationary treatment. Restorative techniques and materials are constantly improving. Regardless of practitioners’ willingness to apply “advanced” techniques, it is mandatory for them to ensure that their efforts do not jeopardize the success of future restorative management. The objective of this paper is to demonstrate the application of this guiding principle in general clinical practice.
Restorative Integrity in Perspective
Restorative integrity depends on the simple relationship between bonds and stress. If the bond can withstand the stress, the restorative technique will be successful.2 The resin-enamel bond strength has proven to be adequate in preventing microleakage and has provided the profession with fairly predictable results since its introduction in 1955.3 Dentin is an entirely different substrate. Kiyomura was the first to draw the profession’s attention to the lack of resin-dentin bond durability.4 He demonstrated a reduction from 18 MPa to 4 MPa after five years of storage in water at 37șC. Nakabayashi and Pashley have recently examined this alarming deterioration and postulated that it was the result of over-etching of the dentin and incomplete resin impregnation of the demineralized layer of dentin.5 This problem resulted in an amorphous layer beneath the hybrid layer consisting of unprotected collagen fibres that hydrolyzed over time.
Clinicians should beware of the remarkably high “in-house” bond strengths reported by bonding resin manufacturers as these “24-hour” tests do not reflect decline over time. No long-term studies have been done on the durability of dentin bonds in vivo. Given the multiple presentation conditions of patients, there is no way to ensure that the chosen bonding system will successfully infiltrate to the complete depth of the demineralized dentin in every case.
In light of the above, it would seem prudent to inform patients of the temporary nature of tooth-coloured restorations and of the various risks, benefits and associated maintenance costs of restorative therapy. The patient may thus more fully realize that the outcome of extensive adhesive restorative procedures is not entirely predictable.
 |
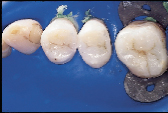
| Figure 2: Post-operative view of the restored fractured distal incisal edge of the right central incisor done without any mechanical tooth preparation. |
Consider, for example, the common occurrence of a fractured incisal edge in a newly erupted central incisor of a child patient. Traditionally, the perimeter of the fractured tooth substance is chamfered to accommodate an increase in the bondable substrate area and to allow for an imperceptible tooth restoration. In many instances, the preparatory procedure removes more sound tooth structure than the initial trauma. This irreversible tooth preparation will affect all future restorative interventions. In the case of the eight-year-old patient depicted in Fig. 2, restoration of the distal incisal edge of the right central incisor was done without the use of any mechanical tooth preparation. The slightly compromised esthetic result (shown 18 months after a second traumatic episode fractured the adjacent lateral incisor) was counterbalanced by the fact that the restoration was done without further loss of sound tooth substance. The restoration should last approximately five years, at which point an improved restorative material will allow for an enhanced esthetic result. This case is illustrative of an evolving restorative mentality that acknowledges:
• the esthetic and structural deficiencies of current technology
• the sacrosanct status of tooth substance and the irreversibility of tooth reduction
• the ongoing improvement of adhesive techniques and materials
• the need to set more realistic expectations by adequately informing patients.
Without appropriate consent, sound tooth substance should not be sacrificed to accommodate esthetics in the posterior dentition, particularly when it is anticipated that the restorative treatment will be redone a number of times throughout an individual’s life.
 |
 |
| Figure 3a: A reattachment procedure for the fractured central incisors was done as an interim treatment option. | Figure 3b: Definitive treatment can be delayed until tooth and gingival maturation is complete. |
The corollary to acknowledging the probationary nature of our restorative efforts is that definitive treatment can justifiably be deferred until tooth and gingival
maturation is complete. The fractured central incisors depicted in Figs. 3a and 3b are representative of this principle. The pulps of both teeth were exposed following a traumatic episode. Following pulp capping using the total etch technique, the fractured incisal tooth fragments were reattached by means of a dentin bonding agent.6 Two and a half years later both teeth are vital, but the reattached fragments are discoloured and the patient is dissatisfied with the visible tooth fragment (Fig. 3a). The reattachment procedure was delivered as an interim treatment that not only maintained the biological seal of the pulpal tissues but also allowed for subsequent preparation of veneers (Fig. 3b).
Clinical Reality of Treatment Selection
The restoration of the primary tooth is the epitome of “obsolescence” as the tooth will likely be replaced before the restoration fails. With the permanent dentition the reverse is true as treatment will likely need to be redone a number of times during an individual’s life. Obviously, the restorative option that will last the longest should be regarded as optimal.
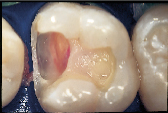
However, many of our restorative options are limited by patients’ financial situation. In cases where patients are forced to forego an ideal indirect restoration, a well-placed, less than ideal direct composite resin may be the best compromise treatment if they are seeking a non-metallic restoration (Figs. 4a and 4b). Consider the depth and width of the lesions of the three maxillary teeth in Fig. 4a. These teeth would be best restored with an indirect option subsequent to the appropriate gingival relocation. Nevertheless, for this patient who requested a tooth-coloured restoration, the challenge was met with innovative procedural manipulations and the diligent application of basic adhesive principles. Sometimes a compromise treatment is the best option in particular circumstances, as long as the decision is reached jointly by the dentist and patient and the latter is informed of all reasonable options.7 In this instance, the patient now has the opportunity to use an indirect approach in approximately eight years time when the restorative margins begin to break down. Without the direct “intermediate” treatment, the teeth may have been further structurally compromised by the expanding and leaking cariously undermined alloys. (It is not the author’s intention to disparage the adhesive process but rather to put restorative expectations in perspective so that the appropriate level of clinical diligence can be maintained. Although improved placement techniques may enhance the performance of current posterior composite resins over their predecessors [ Fig. ], they should still be regarded as a compromised restorative option when applied to extensive lesions.)
 |
 |
 |
 |
| Figure 4a: For patients with limited finances, a well-placed, direct composite resin may be the best compromise treatment if they are seeking a non-metallic restoration | Figure 4b: Post-operative view of restored maxillary sextant. | Figure 5a: A direct composite resin was used for this maxillary first molar since the patient could not afford an indirect solution. | Figure 5b: Esthetics, function and form successfully restored. |
It is fair to say that adhesive dentistry has changed too fast for existing checks and balances, and as a result, clinical success is more difficult to quantify. Although it is tempting to use esthetics as a measure of success, restorative integrity as evidenced by clinical durability should be the true measure of performance. Improvement in materials and innovative clinical applications must continue. In the meantime, current adhesive technology should be regarded as probationary.a
Dr. Liebenberg maintains a private practice in North Vancouver, B.C.
Reprint requests to: Dr. William H. Liebenberg, Suite 201-2609 Westview Dr., North Vancouver, BC V7N 4M2
The author has no declared financial interest in any company manufacturing the types of products mentioned in this article.
1. Liebenberg WH. Partial coverage indirect tooth-colored restorations: steps to clinical success. Am J Dent 1999; 12:201-8.
2. Unterbrink G, Liebenberg WH. Flowable resin composites as “filled adhesives”: literature review and clinical recommendations. Quintessence Int 1999; 30:249-57.
3. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res 1955; 34:849-53.
4. Kiyomura M. Bonding strength to bovine dentin with 4-META/MMA-TBB resin. Long-term stability and influence of water. J Jpn Dent Mater 1987; 6:860-72.
5. Nakabayashi N, Pashley DH. Hybridization of dental hard tissues. Chicago: Quintessence; 1998. p. 57-83.
6. Liebenberg WH. Reattachment of tooth fragments: operative considerations for the repair of anterior teeth. Pract Periodontics Aesthet Dent 1997; 9:761-72; quiz 774.
7. Iacopino AM, Wathen WF. Geriatric prosthodontics: an overview. Part I. Pretreatment considerations. Quintessence Int 1993; 24:259-66.